Medical Delta, the collaboration between TU Delft, Leiden University, LUMC and Erasmus MC Rotterdam, started 12 new projects to develop solutions for sustainable healthcare.
Jenny Dankelman's project Rapid Innovation of Minimally Invasive Instruments is one of twelve that received funding. (Photo: TU Delft)
 Wouter Serdijn: “We will develop a first-of-a-kind arrhythmia-on-a-chip model.” (Photo: Sam Rentmeester)
Wouter Serdijn: “We will develop a first-of-a-kind arrhythmia-on-a-chip model.” (Photo: Sam Rentmeester)
“One of the main problems is that many patients suffering from these brain disorders are diagnosed relatively late. In the current project, we will develop and evaluate a system for mouse models suffering from these types of disorders, paving the way for clinical applications. More specifically, we will develop a device that will allow us to monitor and modulate activity simultaneously in multiple brain regions of freely-moving animals. This will lead to a better understanding of network phenomena in the brain and the development of better treatment modalities for two disorders that lead to deficits in individual and social behavior: migraine and autism.”
The second project Serdijn works on is the Medical Delta Cardiac Arrhythmia Lab
Heart arrhythmia is a group of conditions in which the heartbeat is irregular, too fast, or too slow. The mission of the Medical Delta team is to decrease the cardiac arrhythmia burden by providing patient-tailored therapy. “To this end, we plan to design and test novel bio-electrical diagnostic tools. We will develop a first-of-a-kind arrhythmia-on-a-chip model to study arrhythmia mechanisms, identify novel therapeutic targets and test innovative therapies.”
Heart arrhythmia is a group of conditions in which the heartbeat is irregular, too fast, or too slow. The mission of the Medical Delta Cardiac Arrhythmia Lab is to decrease the cardiac arrhythmia burden by providing patient-tailored therapy. “To this end, we plan to design and test novel bio-electronic diagnostic tools. We will develop a first-of-a-kind arrhythmia-on-a-chip model to study arrhythmia mechanisms, identify novel therapeutic targets and test innovative therapies.”
 Prof. Jenny Dankelman, Head of the Minimally Invasive Surgery & Interventional Techniques (MISIT) group at the Department of Biomechanical Engineering, and colleagues from LUMC and Erasmus MC will develop modular catheters for minimally invasive interventions. (Photo: TU Delft)
Prof. Jenny Dankelman, Head of the Minimally Invasive Surgery & Interventional Techniques (MISIT) group at the Department of Biomechanical Engineering, and colleagues from LUMC and Erasmus MC will develop modular catheters for minimally invasive interventions. (Photo: TU Delft)Getting certification for newly developed surgical instruments is cumbersome. Prof. Jenny Dankelman, Head of the Minimally Invasive Surgery & Interventional Techniques (MISIT) group at the Department of Biomechanical Engineering, and colleagues from LUMC and Erasmus MC will develop modular catheters for minimally invasive interventions. “The idea is to use a modular design approach for catheters in a similar way as we did before for surgical instruments where we used a modular shaft on which grippers, scissors and other tips can be placed,” she says.
Her project aims to cover the complete innovation chain. Dankelman: “We build and test a pipeline for moving a device concept from a first proof-of-principle, through regulatory approval, to clinical evaluation and implementation.”
Besides building instruments, her team will also perform tests on so-called phantoms, which are tissues that mimic real organs and medical abnormalities. Using phantoms for this purpose should aid the process of regulatory approval for new instruments. Phantoms can also replace some animal experiments and clinical trials for instrument testing.
The programmes combine the knowledge and expertise of three universities and two university medical centres to address important societal healthcare challenges such as dementia, helping the elderly stay mobile as long as possible, and the regeneration of tissues with stem cells. They will receive almost EUR 400,000 each. Delta spoke to six of the Delft scientists involved.
 Marco van Vulpen is involved in the project HollandPTC programme on Health Technology Assessment. (Photo: TU Delft)
Marco van Vulpen is involved in the project HollandPTC programme on Health Technology Assessment. (Photo: TU Delft) Due to its very local dose deposition, proton therapy for cancer patients is expected to administer smaller doses to the surrounding healthy tissue, thereby significantly reducing the long term side effects of the current standard of care, photon therapy. “The HollandPTC programme on Health Technology Assessment should result in a model that will determine the cost effectiveness of proton therapy,” says Professor of Radiotherapy, Marco van Vulpen. He is also the medical director of the HollandPTC radiation clinic. Two PhD Students will map the cost structure of the proton centre. Next to this, the value proposition of proton therapy for head, neck and brain tumours will be determined.
The proton clinic HollandPTC was officially opened several weeks ago. Read more about the opening here.
 Associate Professor in Persuasive Game Design, Valentijn Visch: “This proposal aims to develop and evaluate a specially tailored eHealth lifestyle programme.” (Photo: TU Delft)
Associate Professor in Persuasive Game Design, Valentijn Visch: “This proposal aims to develop and evaluate a specially tailored eHealth lifestyle programme.” (Photo: TU Delft)Associate Professor in Persuasive Game Design, Valentijn Visch, of the Faculty of Industrial Design Engineering, is one of the researchers involved in this project related to cardiovascular disease. “Cardiovascular disease is a leading cause of death and disease burden, disproportionately affecting people with lower socio-economic status,” Visch says. “The key to preventing and reducing this disease burden primarily consists of adopting and maintaining a healthy lifestyle. It is especially challenging for people in the lower socio-economic groups to adopt healthy behaviours, making this a vulnerable group and the key focus for intervention approaches. Current lifestyle programmes often fail to reach and motivate this group. This proposal aims to develop and evaluate a specially tailored eHealth lifestyle programme.”
 Professor of Clinical biomechatronics, Jaap Harlaar: “Motor disability is one of society’s main challenges.” (Photo: Jos Wassink)
Professor of Clinical biomechatronics, Jaap Harlaar: “Motor disability is one of society’s main challenges.” (Photo: Jos Wassink) The burden of disabilities due to neurological and joint diseases strongly increases with age. “Given the ageing population, motor disability is one of society’s main challenges,” says Professor of Clinical biomechatronics, Jaap Harlaar, of the Biomechanical Engineering group. “The Improving Mobility with Technology programme combines medical and technological expertise to enhance treatments to improve mobility to promote daily activities”, he says. The research group will develop a portable device with a gyroscope that will help disabled people maintain their balance. The researchers will also use a robotic support system to enhance rehabilitation after a stroke. Furthermore they will develop precision diagnostics for knee osteoarthritis.
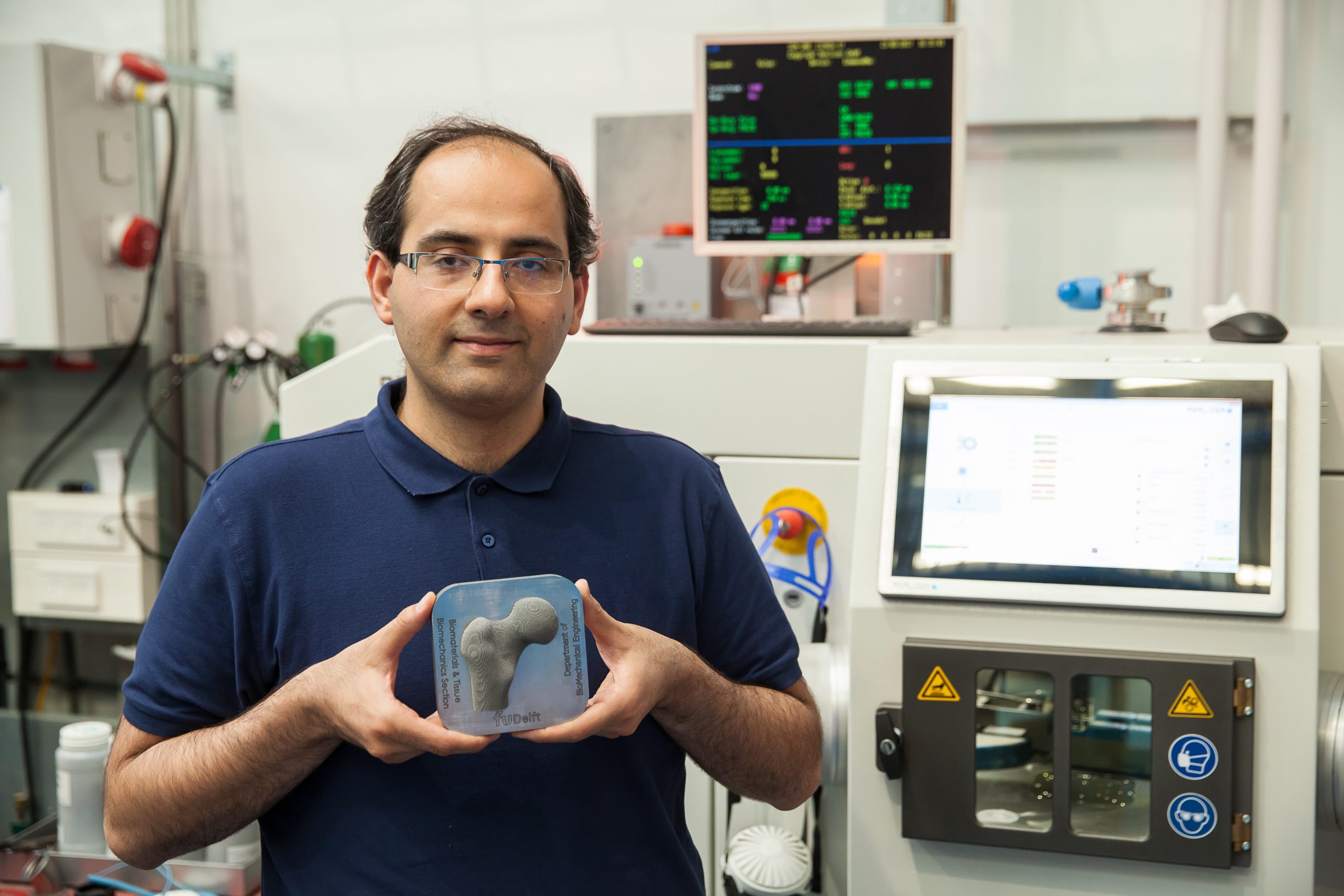 Prof. Amir Zadpoor: “We are focussing on the bone-cartilage interface and liver, which are very complex tissues to regenerate.” (Photo: TU Delft)
Prof. Amir Zadpoor: “We are focussing on the bone-cartilage interface and liver, which are very complex tissues to regenerate.” (Photo: TU Delft)Together with colleagues from Leiden and Rotterdam, Professor Amir Zadpoor (Department of Biomechanics Engineering) is working on tissues and organ systems derived from human stem cells. “We are focussing on the bone-cartilage interface and liver, which are very complex tissues to regenerate. We call our project 4D because we want our 3D biomaterials to be able to change their shape or properties over time.” The applications of the designed tissue constructs include reconstructing osteochondral defects and studying liver diseases using patient-specific mesenchymal and epithelial stem cells.
Neurodelta
Professor Wouter Serdijn of the Faculty of Electrical Engineering, Mathematics and Computer Science is involved in two of the projects. The first is called NeuroDelta: Ambulant Neuromonitoring for Prevention and Treatment of Brain Disease. Brain disorders that involve multiple brain regions are notoriously difficult to treat and impose a huge burden on society. Examples are migraine and autism. The NeuroDelta Consortium will try to tackle these disorders.
 Wouter Serdijn: “We will develop a first-of-a-kind arrhythmia-on-a-chip model.” (Photo: Sam Rentmeester)
Wouter Serdijn: “We will develop a first-of-a-kind arrhythmia-on-a-chip model.” (Photo: Sam Rentmeester)“One of the main problems is that many patients suffering from these brain disorders are diagnosed relatively late. In the current project, we will develop and evaluate a system for mouse models suffering from these types of disorders, paving the way for clinical applications. More specifically, we will develop a device that will allow us to monitor and modulate activity simultaneously in multiple brain regions of freely-moving animals. This will lead to a better understanding of network phenomena in the brain and the development of better treatment modalities for two disorders that lead to deficits in individual and social behavior: migraine and autism.”
The second project Serdijn works on is the Medical Delta Cardiac Arrhythmia Lab
Heart arrhythmia is a group of conditions in which the heartbeat is irregular, too fast, or too slow. The mission of the Medical Delta Cardiac Arrhythmia Lab is to decrease the cardiac arrhythmia burden by providing patient-tailored therapy. “To this end, we plan to design and test novel bio-electronic diagnostic tools. We will develop a first-of-a-kind arrhythmia-on-a-chip model to study arrhythmia mechanisms, identify novel therapeutic targets and test innovative therapies.”
 Prof. Jenny Dankelman, Head of the Minimally Invasive Surgery & Interventional Techniques (MISIT) group at the Department of Biomechanical Engineering, and colleagues from LUMC and Erasmus MC will develop modular catheters for minimally invasive interventions. (Photo: TU Delft)
Prof. Jenny Dankelman, Head of the Minimally Invasive Surgery & Interventional Techniques (MISIT) group at the Department of Biomechanical Engineering, and colleagues from LUMC and Erasmus MC will develop modular catheters for minimally invasive interventions. (Photo: TU Delft)Getting certification for newly developed surgical instruments is cumbersome. Prof. Jenny Dankelman, Head of the Minimally Invasive Surgery & Interventional Techniques (MISIT) group at the Department of Biomechanical Engineering, and colleagues from LUMC and Erasmus MC will develop modular catheters for minimally invasive interventions. “The idea is to use a modular design approach for catheters in a similar way as we did before for surgical instruments where we used a modular shaft on which grippers, scissors and other tips can be placed,” she says.
Her project aims to cover the complete innovation chain. Dankelman: “We build and test a pipeline for moving a device concept from a first proof-of-principle, through regulatory approval, to clinical evaluation and implementation.”
Besides building instruments, her team will also perform tests on so-called phantoms, which are tissues that mimic real organs and medical abnormalities. Using phantoms for this purpose should aid the process of regulatory approval for new instruments. Phantoms can also replace some animal experiments and clinical trials for instrument testing.
Do you have a question or comment about this article?
tomas.vandijk@tudelft.nl


Comments are closed.